Innovative health and wellbeing solutions for today and tomorrow
Health and wellbeing

Health and wellbeing organisations must tackle the complex challenges confronting the industry both now and in the future. At PwC, we support them in achieving this through our combined creativity and an array of human-centered and technology-driven health and wellbeing services.
Our teams draw on both national and global expertise to offer new perspectives and fresh approaches.
We are a dedicated community with a deep, unwavering commitment to serving the Australian people, consistently delivering solutions that are innovative, impactful, and lasting.
Future of care
Innovative solutions for your needs - 4 items
Supporting you across the healthcare industry
Australia’s health and wellbeing sector continues to grapple with entrenched systemic challenges: an ageing population, chronic disease, workforce shortages, financial sustainability concerns, clinical burnout, and stark geographic disparities in access and outcomes.
Together, these forces are creating a complex, high-stakes environment that demands bold thinking, cross-sector collaboration, and a reimagining of how we deliver care.
Australia's growing senior population deserves exceptional care, wellbeing, and fulfillment, achievable through the provision of safe, high-quality, and respectful care services. While the challenges in the aged care sector are significant, there are immense opportunities to revolutionise the delivery of these services.
PwC collaborates with clients and key stakeholders to address these challenges and foster innovation throughout the sector. We unite a remarkable community of problem solvers and experts, all dedicated to transforming ageing and aged care in Australia for the better.

With Australia's ageing population and the rise of chronic diseases, the demand for private hospitals is expected to increase in the coming years. However, financial and operational pressures continue to present hurdles, and workforce shortages are limiting capacity to meet this demand.
To address these challenges, we offer solutions that are human-centred, insight-driven, and digitally enabled, aimed at delivering quality improvement strategies for a more effective healthcare experience.

Private health insurers in Australia are facing a period of uncertainty as rising healthcare costs, shifting demographics, and evolving consumer expectations reshape the sector.
At PwC, we help health insurers through our collective ingenuity and suite of human-led and tech-powered health and wellbeing services, to achieve their business goals.

Australia’s mental health system is under increasing pressure, and the implications for Australia’s economy and productivity are far-reaching.
We are committed to digitally transforming the way mental health and wellbeing services are delivered. We focus on our people, our clients and society more broadly, to enable access to the right care at the right time.

Aligned to PwC’s purpose of solving important problems, we believe that there is much that can be done to deliver better outcomes for people with disabilities, along with their families and carers.
Through data-driven insights, innovation and experience, our disability advisory services team can help you navigate your increasingly complex legal and regulatory obligations into a more certain future.

Australia's pharma and MedTech sectors are poised for continued growth, driven by an ageing population, aged care reforms, rising home-care demand, and bolstered by robust investment and innovation.
Our passionate team of solvers can help you succeed with consulting, assurance, deals, cybersecurity, and sustainability services.

Value in motion
Industries are reshaping around fundamental human needs, creating value through collaboration across interconnected domains that now replace traditional value chains.
Insights direct to your inbox
Hear from the health experts at PwC with news, insights and information about future events.
Meet the team

Health & Education Industry Leader, PwC Australia
Nicola Lynch is a passionate advocate for the transformative roles of health and education in communities, the economy, and the lives of Australians. As a Partner and Leader of our Health & Education Industry team at PwC, she is deeply committed to empowering people by providing purposeful work and opportunities to make meaningful impact.

Health Advisory Leader, Health Economist, PwC Australia
Marty is passionate about improving the health system using health economics frameworks to maximise the value in health funding and to measure return on health investments. In his role as Partner and Health Advisory Leader at PwC, Marty is dedicated to enhancing the effectiveness and efficiency of health, aged care, and disability services.
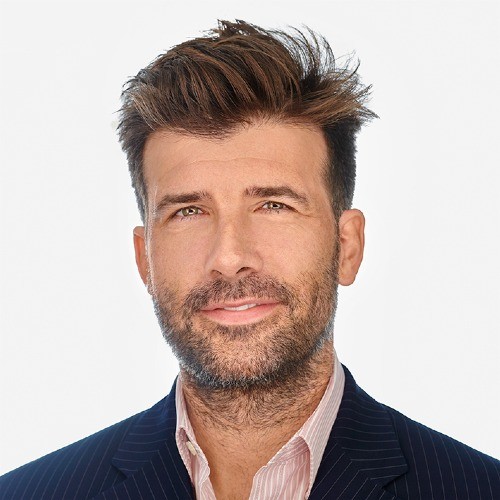
Partner, Advisory, PwC Australia
Alex Micallef-Jones, Partner at PwC and the Private Hospitals Sub-Sector Leader, is dedicated to guiding organisations through complex transformations with innovative solutions that address both immediate needs and long-term goals.

Amy Bryan
Managing Director, PwC Australia
Amy Bryan is dedicated to enhancing governance, risk management, and audit practices within the healthcare sector. With over 12 years of experience, Amy stands out as a trusted advisor in health and aged care, and for delivering robust and sustainable solutions that foster safety and quality care.














